3 Stress Axes: driving health or sickness (with examples and pointers) - Part 1
Apr 29, 2022NB: the following is an excerpt from the new book we are preparing. It will be available in the next few months ... new information ready soon!
There is a lot of talk about stress, both on a personal level, as a problem that almost everyone experiences, and in the various scientific communities. In fact, the stress response (or rather " responses", as we will shortly see) is closely woven into the fabric of life and affects everyone all the time. Modern life often pushes us to the limit, towards wanting to achieve more in our studies, at work or in our other areas of interest. We’re pushed to never stop ("just one more..." is the typical mantra when we’re watching a TV series that fascinates us, or opting for another chocolate, a caress and other things we like), but often the consequences of this behaviour are much more damaging in the long term than they are beneficial in the short term.
Connections between stress, body and emotions
From a scientific perspective, it is a good thing that stress is studied by several disciplines because it is a phenomenon that affects the whole being and that moves on emotional, mental and physical levels driving constant reciprocal influences. Thanks to targeted investigations, it has been possible to discover that there are multiple stress axes (and not, as it was usually taught, a single axis) and to clearly understand the scientific foundations of typical psychosomatic disorders. It is now in fact possible to clearly understand how stress can generate stomach pain, dermatitis, physical or emotional suffering, depression and even serious degenerative diseases. At the same time, the inverse mechanisms, whereby certain bodily conditions can alter mental state and cause emotional distress, are also well understood.
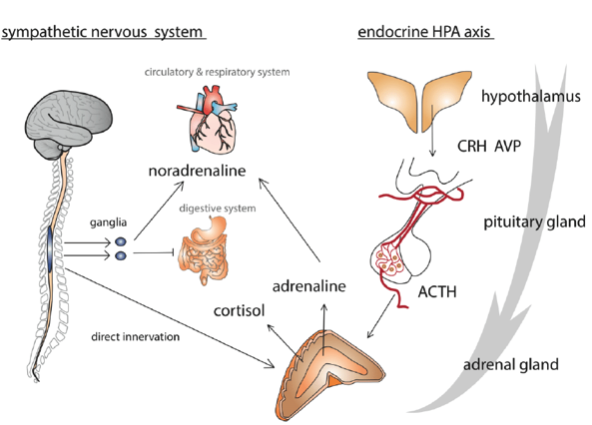
The two main and best known stress axes have direct implications on the respiratory, circulatory and digestive systems. In this simplified representation we can see some of the more direct activation pathways that come into play if stress becomes chronic and there are no recovery or compensation measures. Stress can, in fact, lead to various "stress" disorders, typically including heart attack, colitis, dysbiosis, ulcers, etc. We will see that there are also numerous other ways in which the stress axes alter our physiology and create various dysfunctions.
Recently, research has revealed a close interaction between the nervous and immune systems in the regulation of inflammation that links psychological and social stress with chronic somatic diseases and vice versa. In the short term, stress can save our lives, allow us to adapt, help us overcome new challenges and learn new skills. It is also the basis of various motivational and hedonistic processes: just think of any game or sport and you will find they have all these typical elements in common. In the long run, however, when stress becomes chronic, when we cannot see escape routes or alternatives, there are no opportunities to fight or to reinvent ourselves because we have run out of resources (from the most concrete ones to emotional and social ones) then health pays a price.
To understand these processes and to shed some light on them, let's take a look at the main stress axes. Once these aspects are understood (it is not necessary to know and remember every feature in detail, but it is enough to grasp the general mechanism), the need for an integrated approach immediately becomes clear. We will illustrate the various practical applications that derive from it throughout the book.
The three main axes of stress
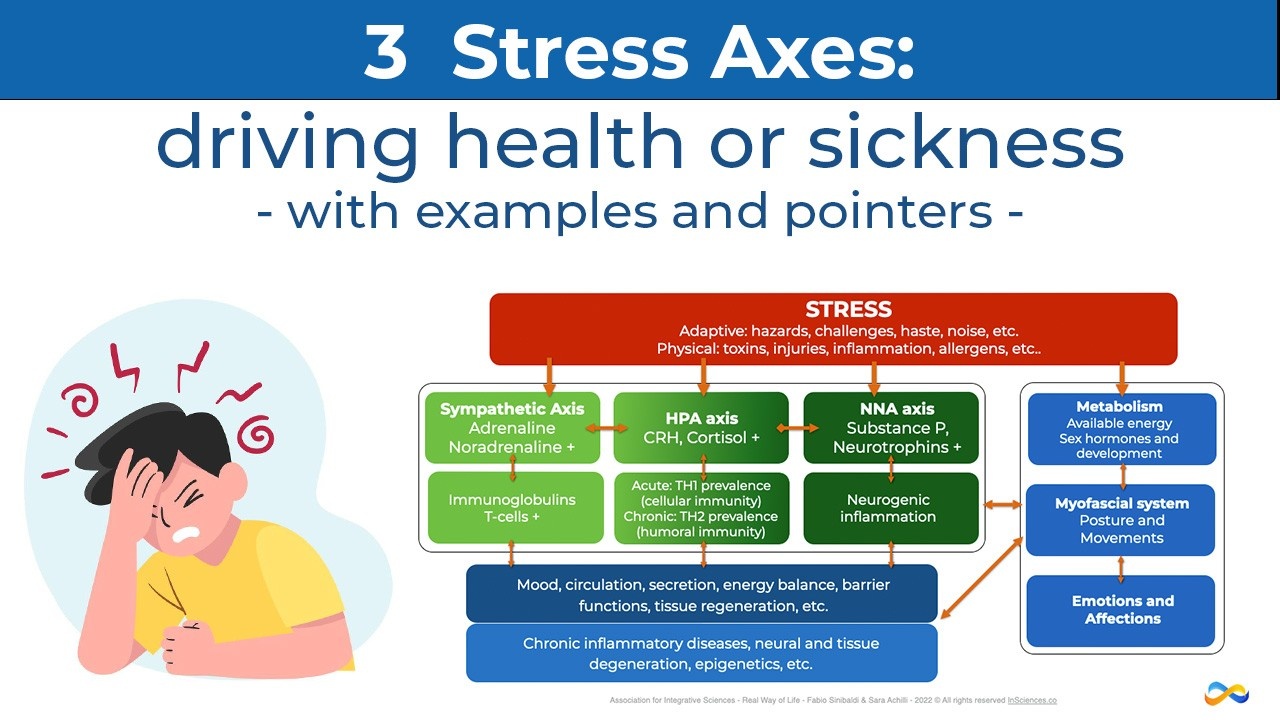
The axes described below are not independent, but act both in parallel and in synergy with each other, exerting reciprocal influence. A clear distinction, however, helps us identify all the different processes that compose them more clearly.

The 3 main stress axes with their interactions and implications in all areas of human life (thoughts, emotions, movement, posture, pathogenesis, etc.).
1 - Sympathetic Axis
In chronological order, the earliest known stress axis is the Sympathetic. Walter Cannon Bradford, with the discovery of norepinephrine in peripheral nerve fibres and of adrenaline derived from the adrenal gland, identified the so-called fight-or-flight response. This nervous system axis triggers the orthosympathetic system (in instances of activation) or, vice versa, makes room for the parasympathetic one (in deactivation instances). Contrary to teaching up to now, the sympathetic and parasympathetic systems, are not opposites and antagonists (an "accelerator and a brake"), but work in synergy.
This axis starts at the hypothalamus, passes through the Locus Caeruleus and works through other organs up to the adrenal glands, in particular the medulla, where it produces adrenaline and noradrenaline (called catecholamines).
It is a well-known fact that the hypothalamus plays a key role in stress responses, integrative processes and numerous self-regulation activities. Although less wide-spread, the notion that the locus caeruleus (LC) also plays a central role on several fronts is also common. In fact, it centrally controls activity and connectivity of all brain areas both directly and indirectly, especially when it comes to the regulation of the prefrontal, motor and sensory areas as well as the limbic cortex. This helps us see clearly that stress responses are all-round reactions on a physical, motor, emotional and mental level. Furthermore, counter-evidence shows that dysfunctions in the connection between the LC and the previously mentioned areas are detectable in any psychiatric or motor disorder.
Noradrenaline, which activates us in the short term, can increase IgE (E immunoglobulin) levels in the long run. These are antibodies that are produced in response to the presence of a stimulus perceived as a potential threat. If the stress reaction is prolonged and not terminated, these excess immunoglobulins give rise to the typical symptoms of sinusitis, asthma, dermatitis, etc. In the long run, an excess in norepinephrine drives neurons to induce mast cells to degranulate histamines, thus favouring allergic reactions.
Peter’s case
Peter is 6 years old and was sent to therapy on the recommendation of his teachers who see him as a worked-up and restless child. His mother confesses that he "is so worked-up that he can’t tolerate anything; sometimes he scratches his arms until they bleed". Peter also has some allergies and intolerances, but his mother doesn’t see this as a problem; she says: "nowadays it’s a very common issue, in fact, who doesn’t have allergies?!".
Unfortunately, the mother is right on this last point: far too many people have immune problems that manifest through allergies and intolerances. Excessive levels of stress, which are now common in our culture, are one of the primary reasons. There are of course also other environmental aspects (pollution and endocrine disruptors), drug abuse, pro-inflammatory nutrition and other elements that we will see in due course. Accepting that it is normal to have problems with intolerances and allergies just because it is widespread is a serious mistake. Let us remember that the norm (hence 'normal') is a statistical criterion for the frequency of an event, it does not mean that it is okay.
In Peter’s specific case, it is enough to observe him while he plays in the waiting room and to talk to him about his interests to see that there are no negative thoughts or worries in his mind. He is a child whose face and words exude serenity. But he seems to be in a body that fits him too tight, like an old outfit: he constantly fidgets, tugs at the neck of his shirt and, at a certain point, begins to scratch himself energetically. I ask him why he does it and he replies that it itches so much, that scratching gives him relief, so much so that he goes on, even though he hurts himself and he knows that his mother and father will scold him for it.
It doesn’t take an expert dermatologist to immediately notice that his skin is extremely dry on his arms, but also a little dry on the rest of the body. Precisely because I am not a dermatologist, I know that plan B, after the necessary tests and checks, is to send him to a specialist. But plan A is as follow: first of all, try to verify or falsify my hypothesis. I explain to Peter and his mother that maybe he is not anxious, but he really does feel a great urge to itch, so they should try applying a common moisturizer (so long as of good quality) over the next few days and see if itching improves and, consequently, reduces the nervousness induced by the itching, pain and a sense of helplessness towards this symptom. This makes Peter immediately feel understood; someone finally offers him an explanation and does not tell him that "he has a problem". Also, he now knows that he doesn't have to feel guilty about his parents, and this removes an additional source of stress.
As we noted earlier, chronic stress releases histamines and promotes allergic reactions. If this is Peter’s case (we are only making a hypothesis, but we can verify it in a simple way), by reducing stress and reducing histamine-rich foods (cured meats, canned foods, strawberries, etc.), we would expect a reduction in symptoms. To temporarily reduce stress, by talking to mum, we decide to suspend violin lessons for a week (which he does not like very much, but his parents push him to attend), to avoid football training (which he does like, but where he is teased sometimes badly).
4 days later, the mother writes to me announcing a miracle: she says that Peter is now a peaceful child and that he no longer scratches himself. Obviously, no miracle has occurred, but we have identified a fundamental element relating to the start of the problem. As a result, using further anti-inflammatory (switch 2) and metabolic (switch 1) measures, we have helped Peter find a balance between duties and pleasures in relation with his parents’ wishes (the violin but not just that, switch 4) and to help manage the kids who made fun of him (both on a communicative-relational level, and working on his confidence at a mental and physical level Switch 3).

- End of part 1
In the next article:
Triggers, Terminations and Recovery of the Sympathetic axis
-
Immune system imbalances in acute and chronic stress
-
The HPA axis - updates
-
All the effects of cortisol
-
Annalisa’s case: perfect therapies are not successful and how to solve the situation
-
The NNA axis and neurogenic inflammation
-
The key role of neurotrophins in various psychosomatic processes
Stay connected with news and updates!
Join our mailing list to receive the latest news and updates from our team.
Don't worry, your information will not be shared.
We hate SPAM. We will never sell your information, for any reason.

